Blowing Up the Ambulance Industry

Today we’re taking about ambulances and the ambulance industry! We know this topic is important because Michael Bay recently released an action movie called… “Ambulance.” This is the director who brings you about 90% of big-budget Hollywood films where car chases happen and lots of shit blows up. And sometimes robots from outer-space. Like a lot of our healthcare system, the ambulance industry has become increasingly privatized, and taken over by for-profit equity firms. This has a dramatic impact on the patients who need emergency medical services (EMS) – often at their most vulnerable moments – as well as the EMS providers who work in the industry, and are increasingly squeezed by their employers.
Podcast: Play in new window | Download
Subscribe: More
Show Notes
Today’s guests are:
J. Wesley “Wes” Boyd, MD, PhD is a professor of psychiatry and medical ethics at Baylor College of Medicine. He is also a Lecturer on Global Health and Social Medicine at Harvard Medical School. Wes has written about and taught extensively in the humanities, medical ethics, human rights and psychiatry.
Aditya Shekhar studies the epidemiology of various emergency medical conditions, including cardiac arrest and traumatic injury. He has contributed to numerous publications in leading medical journals, and his work has been featured by several medical societies. He also has field experience as an emergency medical services (EMS) provider and teaches EMS in the United States and internationally.
Wes and Aditya published an article in Slate: “Ambulance Raises an Important Point About Ambulances; The box office flop is basically a commercial for Falck, a for-profit ambulance company with slow response times.”
As research for this podcast, Gillian watched the movie Ambulance. (Thank you for your service Gillian.) The movie actually realistically depicts the failure of our healthcare system. Our hero, whose insurance company denies coverage for his wife’s life-saving treatment, robs a bank and abducts an EMT, using an ambulance as a getaway vehicle. (What? It could happen.)
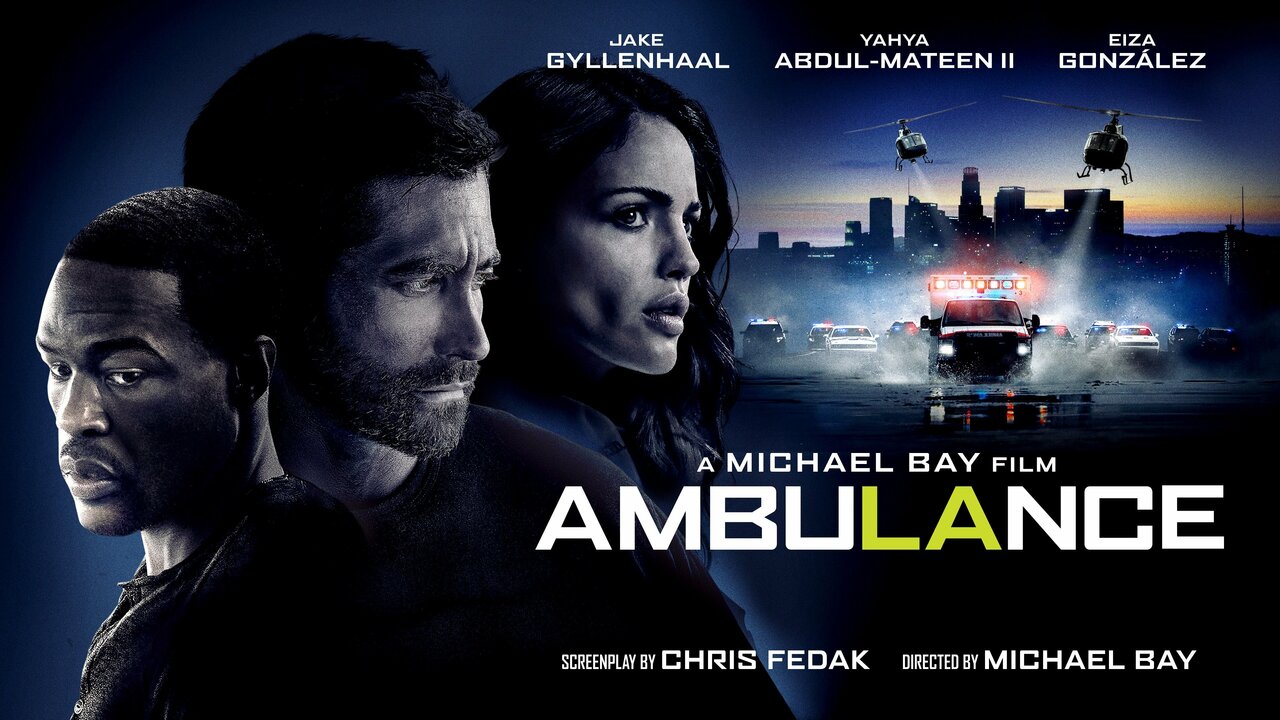
Aditya shares how his experience in EMS is and is not like the movie. For example, unlike the movie, EMS providers don’t typically perform surgery in an ambulance. He has also never been kidnapped by Jake Gyllenhaal. But they do provide care in the moment a patient is at their most vulnerable, helping them get to the most appropriate care.
Wes describes his experience working in an outpatient psychiatric clinic, about a mile and a half away from a hospital. He crossed paths with EMS whenever a patient was at risk of self-harm, when he would have the patient transported to the Emergency Room. Many patients begged him not to call the ambulance and let them get themselves to the ER, because previous ambulance trips came with a bill of over $2,000. At one point he even drove the patient to the ER himself to avoid that expense.
Ambulance services are increasingly becoming privatized. The trend sped up after the 2008 economic crisis because cities struggled to afford these services. Many of these companies are owned by private equity firms, who saw an opportunity to use existing resources to minimize management, while billing the patient’s insurance for high profit.
When a city runs an ambulance service, the goal is to break even, and when they don’t, the city absorbs the cost because it’s a public service the community needs. When a private equity firm runs an ambulance service, the goal is profit, so they cut services, overwork and underpay their staff, and ultimately provide less safe care.
We hear a lot about “surprise billing” in the hospital setting, but surprise billing is also rampant in emergency medical services. Congress recently passed “The No Surprises Act” to address surprise billing, but it has some major gaps when it comes to EMS care.
When patients are in crisis, they are not likely to comparison shop; while some decline EMS care due to cost, often they do not have the capacity to make that choice or seek another option. When a patient must be cared for by the EMS provider that shows up, they’re exposed to surprise billing.
Frontline EMS providers are very disconnected from the billing aspect of the service; much like a doctor can’t tell you how much a procedure is going to cost, the EMS provider probably can’t tell you how much their services will cost. The complicated system of insurance plans and networks (both for hospitals and ambulance services) makes it nearly impossible for an EMS provider to know what the ultimate cost to the patient will be.
With this lack of clarity around billing, many Americans just choose not to take ambulances, using any alternative they can. Obviously this is a dangerous delay of care; if you’re using another form of transportation to the hospital, you’re not getting the care from trained EMS workers on the way, potentially leading to worse outcomes (and bigger bills) in the end.
If a patient needs to be transported from a small community hospital to a specialized facility far from home – for example a rural patient having a stroke would need to go to a comprehensive stroke center, usually only found in larger population centers – a helicopter would be dispatched to bring the patient to the appropriate place for them to receive care. Aditya describes air ambulance services as the wild west. While the number of ground ambulances have declined, the number of air ambulances has ballooned. There’s relatively few restrictions and wide latitude for air ambulance companies to charge whatever they want. Aditya has seen bills for as much as $50,000 or $60,000.
When private equity firms are involved in medicine – in EMS or any other healthcare service – they will do everything they can to maximize profit and skimp on services. Wes describes one private equity firm that owned both a mental healthcare company as well as R. J. Reynolds, the second largest tobacco company in the U.S. and a corporation that is responsible for the number one cause of preventable death in the nation. They are only concerned with profit, not the health of their customers.
Aditya tells us about the No Surprises Act, passed by Congress in order to protect patients from surprise bills due to emergency out-of-network care. Interestingly, ground ambulances were excluded from this legislation (though air ambulances are covered.) We’re waiting to see how the Act is implemented, but it’s unclear who will determine if the care in question was “medically necessary” and thus covered by the legislation. The patient and the provider often don’t know if a situation is an emergency right away, for example a patient with a severe headache; without performing examinations and tests it’s impossible to know if the patient has a life-threatening condition like a tumor, or a painful but non-life-threatening migraine.
Would Medicare for All change the ambulance industry? While it wouldn’t necessarily fix all the ills with EMS companies, removing the profit motive from ambulance services would certainly result in better care and less financial worry for patients.
Resources
- “Ambulance Raises an Important Point About Ambulances: the box office flop is basically a commercial for Falck, a for-profit ambulance company with slow response times.“ Slate.com
- “Why is taking an ambulance so expensive in the United States?” (cnbc.com)
- “Does insurance cover ambulance services?” (thebalance.com)
- If you’re interested in the Black History behind the origin of ambulance services, our shownotes writer would like to recommend learning about the Freedom House Ambulance Service, founded by and for the Black community of Pittsburgh in 1967. Freedom House set the standard for EMS services, for the first time providing emergency care by trained healthcare workers while transporting a patient to the hospital.
Follow & Support the Pod!
You can listen to Medicare for All on Apple Podcasts, Google Podcasts, or visit our website here.
Please donate to the Healthcare-NOW Education Fund to support the podcast!
